Electronic Visit Verification: Common Mistakes and the Right Solutions

How the right EVV solution can improve care outcomes and documentation compliance while meeting your Medicaid reimbursement requirements.
Even though you have been managing complications and challenges during the COVID-19 pandemic, the future of your agency’s reimbursement success relies on your ability to adopt the latest Electronic Visit Verification (EVV) regulations. EVV is new to most providers, and, as with any change, it can feel overwhelming or confusing. Fortunately, by committing to a successful EVV transition with the right solution, you will find EVV can positively contribute to your agency—from quicker reimbursement to better care outcomes.
Unfortunately, many providers have struggled with EVV implementation for one reason or another. Some have struggled to find the right technology that is not too confusing for caregivers to implement, while others find training their staff members is difficult. If you find yourself struggling with the EVV transition, uncovering the right technology can make the transition a success.
More About Electronic Visit Verification
Electronic Visit Verification is a part of the 21st Century Cures Act, which was signed into federal law in December of 2016. The goals of EVV are rooted in better patient care, while providing a new way to decrease fraud, waste, and abuse. EVV is designed to ensure timely service delivery as well as giving agencies a way to monitor services in real-time. Perhaps most importantly, EVV is now required for Medicaid reimbursement.
While EVV was a part of that 2016 federal law, there was a gap between the law being signed and when providers would need to make EVV happen at their agencies. That brings us to where we are today.
Electronic Visit Verification ensures that providers are detailing the services they give at the patient’s home, at the point of care. In order to be reimbursed through Medicare, providers must use EVV to document and report these services through real-time clocking in and out. Caregivers or other providers will be required to document certain data points, including date and time of service, the service provided, the individual receiving the service, the individual providing the service, how long the service was provided and where the service was provided.
While the Cures Act is a federal law, states have been a part of the slower roll-out of EVV. Unfortunately, states that do not enforce EVV federal regulations beginning on January 1, 2021, will be subject to a reduction in federal funding, including Medicaid reimbursement.
Common Mistakes
Electronic Visit Verification has been quite confusing for most home care providers, and for good reason. There have been significant gaps in training for providers from states, and the federal law can be puzzling. Here are a few common mistakes happening around the country, along with some ways you can avoid them.
Not being clear on EVV implementation deadlines.
Perhaps the most confusing part of implementing EVV has been the confusion surrounding when it needs to get done. Current guidance states Personal Care Services (PCS) will need to begin EVV by January 1, 2021. Home Health Care Services (HHCS) must begin by January 1, 2023.
Waiting to think about EVV until it’s too late.
While it can be tempting for many HHCS providers to wait to implement EVV, it is not a wise move. Many HHCS providers give services that are bound by EVV, and they can lose out on federal and state funding or Medicaid reimbursement by waiting to implement the process.
Not researching technology.
Electronic Visit Verification does offer providers the flexibility they need to choose a platform or option that works best for their budget and their caregivers. However, some providers are not doing their due diligence in researching technology options for EVV that could best serve them and their agency in the long run. Instead, providers are implementing solutions that are much too complex for a smooth roll-out, confusing caregivers instead of empowering them.
Not using EVV as a way to positively impact services and patient outcomes.
While transitioning to EVV is a significant change and stressor, some providers are not seeing how EVV can help improve patient outcomes and quality of care. EVV will help to improve caregiver and provider documentation, helping managers to notice trends easier and make adjustments as needed.
Solutions to Look For
No matter if you are playing catch-up with EVV compliance or if you are simply researching a better option to implement at your agency, here are a few considerations to keep in mind as you look at potential platforms.
User-friendly mobile experience
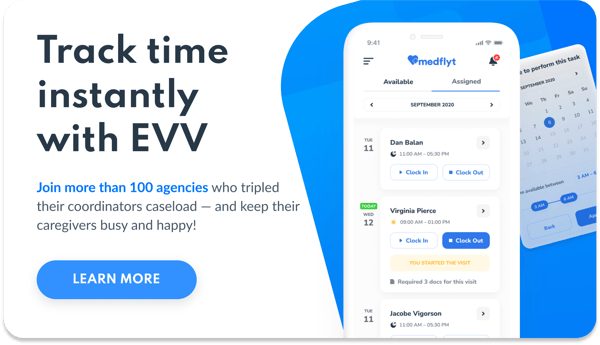
The first test of any EVV solution is if the agency’s caregivers will actually use it. In order for caregivers to use EVV technology, it needs to be seamless and easy to navigate quickly throughout their shift.
Caregivers prefer to use their smartphones to complete their documentation. The right platform should offer an app works with Apple and Android products, making it easy to use. Caregivers should be able to clock in and out digitally with an app that verifies their location via GPS as well as complete documentation requests right on their smartphone.

| Case managers should be able to monitor documentation as well as when caregivers are clocking in or out, in real-time |
Automated push notifications
Caregivers should receive live automated reminders to clock in and out per their schedule, as well as to complete required documentation, with the right platform. These push notifications are just what busy caregivers need to ensure they are completing their EVV requirements.
Further, schedulers or agency leaders should be able to monitor documentation as well as when caregivers are clocking in or out, in real-time. Look for a solution that offers an easy to use dashboard that gives you updated information on who is working where and when, as well as who didn’t clock in for the day, in order to eliminate confusion and make schedule changes even easier.
Documentation reminders
Electronic Visit Verification requires certain data points to be documented every time a caregiver or provider is in the patient home. Find a solution that offers an app for caregivers that prompts correct data point documentation and follow up.
Fast and easy agency-wide implementation
The right solution should have minimal hardware requirements to make the onboarding process as easy as possible. Find a platform that will set your entire agency up digitally in just a few hours.
eMedNY and EVV
If your agency is located in New York, you need to search for an EVV solution that meets eMedNY expectations without doubling your work or caregiver documentation. Currently, the New York Department of Health will utilize the existing Medicaid Management Information System, or MMIS, to collect all EVV data. This means, providers must ensure that their EVV system is able to submit all data points to eMedNY in the specified format in order for the record to be successfully stored in the system.
State Aggregators and EVV
In order for EVV to work, your state needs to receive EVV data points in real-time. This means that your EVV process will need to include a way for you to get the data to your state’s preferred aggregator.
Each state has a different system and depending on where you are located, you will need to work with your state’s preferred system. Common systems include eMedNY, Tellus, and Sandata. Make sure that the EVV solution you are choosing is compliant with your state aggregator.
Subscribe to updates!


